My life changed forever the day that my mother received her leukemia diagnosis. At least, I thought, Mama’s job will come through for her. For the decade prior, my mother had been working in health insurance. While we processed the difficult news, my family assumed that my mother’s job-secured healthcare plan would support her throughout her course of treatment. We were unprepared for the bleak reality.
When she received her diagnosis, my mother had started a 90-day probation period at a new position for one of the top U.S. insurance companies. Her old job’s insurance was no longer in effect. And as the Affordable Care Act hadn’t yet been signed into law — this wouldn’t happen until 2014, six years after my mother’s diagnosis — her case fell under the qualification of a “pre-existing condition.” She was denied the private insurance plan and benefits from her new employer, and had to default to Medicaid.
Given the advanced stage of her cancer, my mother would need specialized treatment to give her a fighting chance. But she was out of network for all specialized cancer hospitals under her Medicaid plan, and would have faced staggering out-of-pocket costs in order to be treated at the top local cancer facility in New York. Instead, she had to face her leukemia battle with a subpar quality of care.
Maybe she would have survived if she had been able to afford a hospital that specialized in cancer treatment. Instead, when her condition deteriorated, she was admitted into an in-network hospital specializing only in trauma.
Maybe she would have survived if we had been able to meet with her oncologist — who only made the rounds at 7 a.m., when I was at work — to talk about available options. As it was, I could barely get attending physicians to share information about her treatment plan. Even when I visited the facility after work, frequently finding my mom disoriented, I had to plead with nurses, tears streaming down my face, to check on her.
Maybe she would have survived if her specimens hadn’t been lost after an important test, delaying further follow-up care and treatment. They never did find those specimens.
Maybe she would have survived if her insurance plan would have afforded her a private room. After all, chemotherapy weakened her immune system, making shared spaces dangerous. But Medicaid meant she couldn’t afford one, leaving her to struggle with recurring infections.
It didn’t matter that my mom and I had worked in the healthcare field our entire careers. Our hands were tied when her cancer was classified as a pre-existing condition, simply because she went to the doctor a few weeks too early. She died in February 2009.
Inequity and the U.S. Healthcare System
I’m certain you’ve heard healthcare horror stories like mine before. Perhaps, you might have a story of your own. For the average person of average means, American healthcare can feel more like a roulette wheel than a system sincerely designed to provide care. The stakes are far, far higher if you are Black or Latinx.
As a young Afro-Latina girl growing up in the Bronx, I dreamed of becoming a doctor. I quickly understood that the healthcare industry didn’t have space for people like me. I often found myself the only young woman of color in these circles. I felt the pressure to conform in order to fit in, at times presenting a whitewashed, muted version of myself. When my mom died, I resolved to take what I’d learned from my job and what I’d lived through to change the future of healthcare for people of color. I knew my approach would have to be radical. I drew inspiration from the history of my community in the South Bronx and from the healthcare activism of the Young Lords and the Black Panthers.
Healthcare inequity for people of color results from several intersecting issues, each layered and complex. People of color face higher rates of, and deaths from, cancer; higher average blood pressures; more instances of infant and maternal mortality; and more diagnoses of diabetes, hypertension and obesity per capita. Moreover, due to generational distrust of racism in medical institutions, people from historically marginalized communities tend to ask fewer questions of doctors. This often leads to more frequent misdiagnoses and a lower overall quality of care.
During the pandemic, this public health crisis grew exponentially more dire, especially within the Latinx community. While Latinx people make up only 18 percent of the U.S. population, the CDC estimates they account for roughly 29 percent of COVID cases nationwide. Latinx individuals contracted over half of California’s COVID cases, despite making up only 39% of state residents. And in New York City, the Latinx community has the highest number of COVID cases and deaths per 100,000 people of any ethnic group.
Healthcare Fluency
If we want to improve the quality of Latinx healthcare in 2021 and beyond, it’s crucial that our solutions address the systemic healthcare inequities that plague all communities of color. Tackling healthcare inequity will be difficult, but it’s not impossible. The key lies in building what I call Healthcare Fluency.
Anyone who is bilingual in Spanish knows there is a major difference between holding a basic conversation and being fluent. The same is true for healthcare. We can practice self-care, go get check-ups and follow the directions to sign up for our employer’s health insurance, but how many of us actually have a plan when there’s an emergency? Not many.
In order to create true healthcare equity for individuals of color, we must take a comprehensive approach — covering all four pillars of Healthcare Fluency: Fundamental Literacy, Scientific Knowledge, Cultural Perception and Personal Confidence.
Fundamental Literacy involves the ability to read, write and speak in the primary language used by a healthcare system. Literacy allows us to fill out medical forms, read our prescription instructions to take the correct dosage, and communicate with our healthcare providers.
Scientific Knowledge speaks to an informed understanding of science, anatomy, medical procedures and, generally, one’s rights within the healthcare system. Without such knowledge, a patient cannot give informed medical consent* to procedures such as hip replacements or vaccines. They may not know how to ask follow-up questions of their healthcare provider.
*It’s important to define informed medical consent as presented by the American Medical Association. Giving informed medical consent as a patient doesn’t mean that you need to have gone to medical school, or even that you need to understand the specific science behind, say, the development of an mRNA vaccine. Rather, the ability to give informed medical consent means that you can understand the diagnosis you have been given, that you understand the nature of recommended treatments and/or interventions, and the multiple outcomes (burdens, risks, or benefits) of all options, including forgoing treatment, so that you can make an informed decision about your healthcare options.
Cultural Perception of the healthcare system comes from the beliefs and information passed on to a patient by their family, friends and coworkers, as well as by other influential figures. If people around the patient are mistrustful of the healthcare system, or of a specific procedure, that will influence the patient’s opinion.
Let’s consider the early stages of COVID, when the CDC said that healthy people didn’t need masks, and limited-supply N95 masks were only important for healthcare providers. Confusion about this guidance, combined with broader fear of the virus, created a perfect storm of “panic buying” and hoarding of N95 masks and respirators (and also toilet paper, of all things). That’s cultural perception, y’all. The current politicization of masks? Also cultural perception. The rumor that vaccines cause autism in children? Yep, you guessed it — cultural perception. The articles you see online or the Facebook posts your tía forwards to you all contribute to this.
Finally, Personal Confidence in the healthcare system is influenced by a patient’s individual trust of the system, including how comfortable they feel advocating for themselves in seeking the right care at the right time. When someone fears or mistrusts the system, they are more likely to avoid the doctor or seek to self-medicate.
Cultural Perception influences Personal Confidence, and these two factors together determine whether someone feels empowered in their healthcare journey. Folks who feel more confident and have trust in the healthcare system are more likely to proactively go to the doctor, ask followup questions about their treatment, and advocate for their personal needs when working with healthcare providers.
Implementation
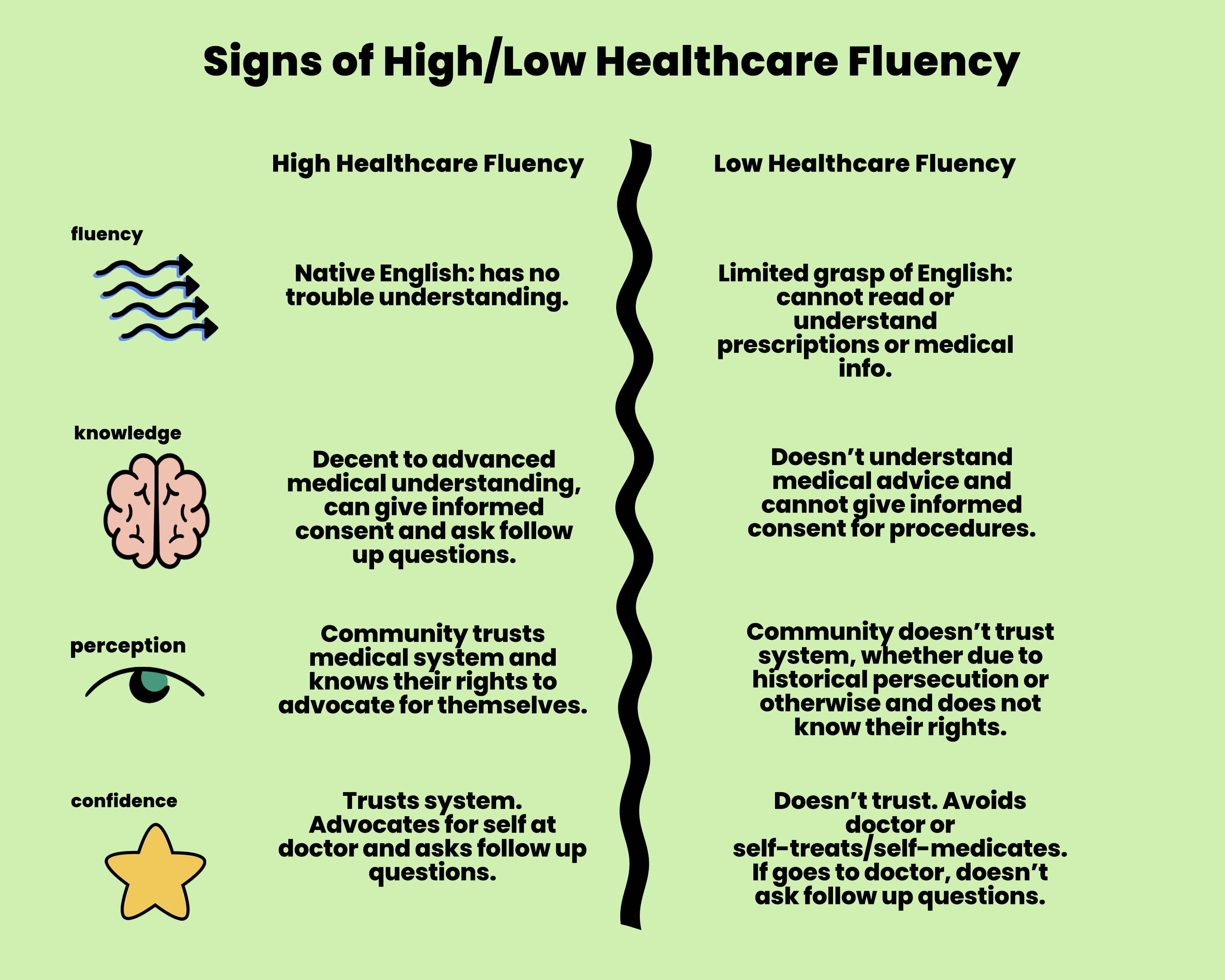
The Latinx community will be better equipped to demand the care we deserve when we increase our ability to speak the language of healthcare and learn our rights. Yet, not everyone’s experience of healthcare fluency looks the same. Let’s consider what those four key areas of healthcare fluency look like in the healthcare journeys of two different folks. I’ll pose two hypothetical scenarios.
Hypothetical A
Carmen, 65 years old, struggles with intense hip pain and is considering a hip replacement procedure.
She is a native Spanish speaker whose Fundamental Literacy in English is limited. She’s been to this doctor before, but she can’t read the prescription instructions or decipher the health insurance rules. When her provider asks her questions, she nods even though she doesn’t understand or gives one-word answers. The language barrier prevents her from understanding fully, and she doesn’t know she can request a translator for her appointments.
Because she was unable to ask more clarifying questions, Carmen has little to no Scientific Knowledge about the full diagnosis, procedure options, or the risks or benefits to completing her procedure. Technically, she is not able to give informed medical consent.
Carmen’s Cultural Perception of the American healthcare system has been negatively affected by others around her. She is generally distrustful of the medical system after hearing stories from her mother about mistreatment during her pregnancy, when she first moved to the U.S. So far, she has been self-medicating for her own hip pain with homemade recipes and natural remedies passed down from her abuela.
Carmen’s Personal Confidence in the healthcare system is very low. She is terrified of the doctor and knows that she might incur a massive bill during her hip replacement. She doesn’t trust prescription medications after losing her husband to an opioid overdose, and she is afraid of becoming hooked on pain pills.
As a result, Carmen decides not to move forward with the procedure and instead simply endures the long term pain.
Hypothetical B
Marisa is a 35-year-old immunocompromised nurse reluctant to receive the COVID-19 vaccine.
Unlike Carmen, Marisa has a high level of Fundamental Literacy and Scientific Knowledge because she speaks English fluently and works in the medical field. But she is still struggling when it comes to Cultural Perception and Personal Confidence. Although she’s a part of the healthcare community and knowledgeable about the vaccine’s side effects, she and the other nurses at her hospital are skeptical about the shot after reading and sharing misinformation posted on Facebook. Marisa does not trust this new vaccine and believes it is politically motivated rather than backed by science. Despite her high risk of contracting a deadly case of COVID-19, Marisa decides against getting the vaccine.
It’s important to make the point here that I’m not passing judgement on Carmen and Marisa for feeling the way they do about the healthcare system. Healthcare Fluency is not about “right” or “wrong.” Their stories simply illustrate how, across educational backgrounds and literacy levels, Cultural Perception of healthcare and Personal Confidence in the system impact how we ask for and receive the care that we need.
Providers need to know how a patient’s own customs, and beliefs will influence how they navigate the healthcare system, or they won’t be able to connect. After all, you can’t give someone a vaccine if they don’t show up for it in the first place.

Two participants in a Radical Health Community Circle. Photography courtesy of Corey Torpie
The Nexus of Healthcare and Comunidad
There’s another key reason why most approaches to healthcare don’t work for much of the Latinx population in America. While our identities and experiences are not singular, as much of the media might suggest, many of our cultural experiences do stem from a strong sense of comunidad.
It doesn’t matter whether we’re eating mofongo or tamales; dancing to the bachata, salsa or mambo; rolling our rr-s or turning them into j-s — Latinx folks often share a spirit of community-mindedness. There is a theme of togetherness and pride in the stories we share and the communal knowledge we pass down. When we are sick, our families often come together to care for one another. It should come as no surprise that Latinx individuals disproportionately take caregiving jobs.

Participants attending a Radical Health Community Circle. Photography courtesy of Corey Torpie
The American healthcare system, in contrast, does not offer community. In fact, healthcare journeys are often isolating experiences. That’s why I knew that the healthcare solution for my community was going to be created from the inside out, not from the outside in.
In 2015, I started inviting an array of healthcare stakeholders — patients, teachers, doctors, nurses and abuelas alike — to have a seat at the table (quite literally, my kitchen table) for a conversation. We leaned on each others’ lived experiences to imagine a new system of healthcare, accessible and equitable for everyone.

Radical Health’s 3 Step Plan
The result was Radical Health, my organization in the South Bronx. We facilitate communal discussion using traditional indigenous conversation-circle practices, then share that data with public health organizations to make systemic, positive change. Unlike traditional approaches that focus only on Fundamental Literacy and Scientific Knowledge, Radical Health bridges those elements by also addressing Cultural Perception and Personal Confidence.
In turn, Radical Health doesn’t provide clinical support, but rather addresses inequality in two ways: engaging the community and equipping patients to navigate the medical system. To accomplish the latter, we provide education to help folks understand their diagnoses, manage their health status and ask important questions. One of our most popular support services is our text-based Radical Relay app that helps patients learn their healthcare rights. Additionally, our work extends into multiple healthcare spheres, from pregnancy and postnatal care to opioid addiction and environmental pollution effects.
In the six years since we incorporated, we’ve hosted more than 3,255 hours of people-to-people listening sessions. This hyper-local approach has proved successful in projects like the Bronx Action Plan. Just like my kitchen table conversation back in 2015, our restorative health circles garnered firsthand accounts from community members, doctors and neighborhood leaders.
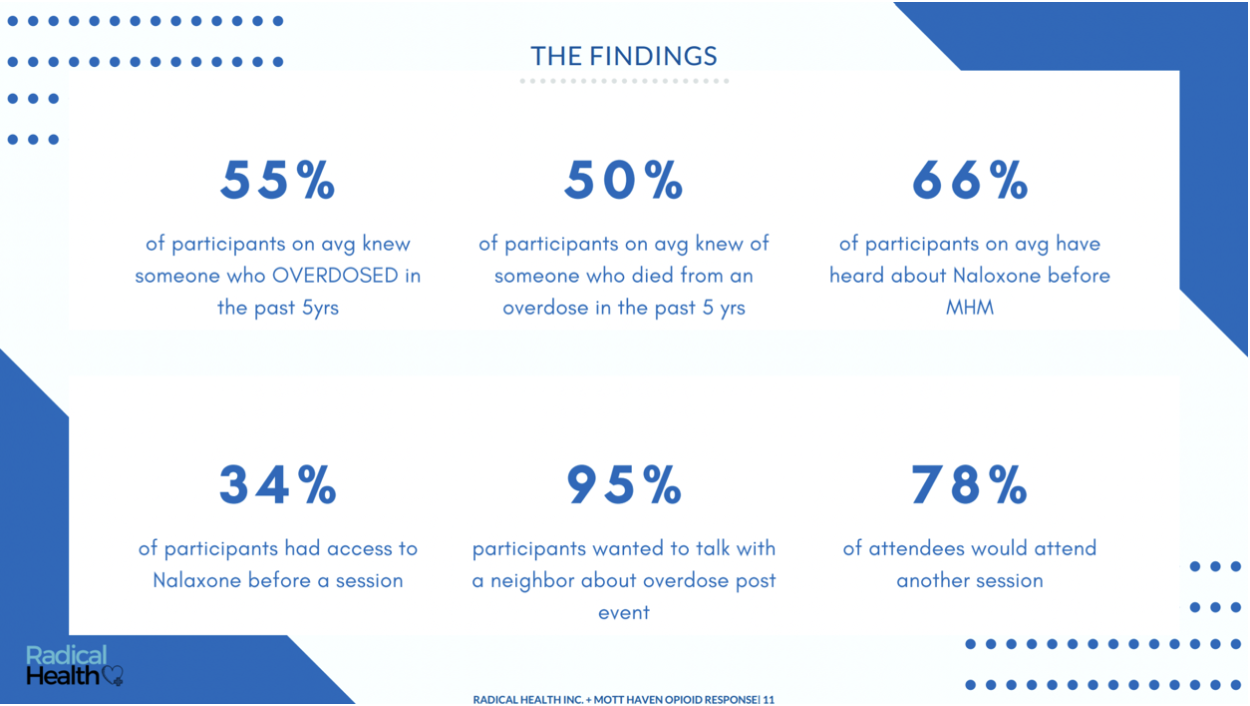
A snapshot of Radical Health’s restorative health circle findings
Using our proprietary data analysis system, we used the information collected in these circles to assist the New York City Housing Authority and the New York City Health Department to identify critical gaps in the local healthcare system. Ultimately, we chose to implement the Action Plan in a Bronx community hit hard by the opioid epidemic. We distributed hundreds of Narcan kits, and equipped countless users with resources, information and support to help prevent overdose deaths.
Conclusion
Would my mother have survived cancer if she had been more fluent in the healthcare system? If she had been able to afford the cost of experimental treatments, or care at a hospital specializing in leukemia? I cannot say for certain. What is certain to me, though, is that all the obstacles in her way made it so she didn’t even stand a chance.
When you know the rules and trust the system, you’re more likely to ask questions and expand your knowledge about your health. Empowering people to achieve Healthcare Fluency is an integral goal of Radical Health’s mission for health equity. The language of the healthcare system is complicated, and there are very few who fully understand how to navigate it. In fact, 77 million people in the U.S. reported that they don’t understand basic health information — and it’s costing our system billions of dollars each year!
It doesn’t matter if we’re considering a hip replacement, planning to have a baby, or worrying about getting a vaccine — a lack of Healthcare Fluency will almost certainly hurt our ability to get the care we need and deserve. As we think about the future of healthcare for Latinx people and other people of color, the worst scenario for us is to continue to be silent, unaware of our rights.
That is why transforming the healthcare system ultimately depends on meaningful, organic conversations. You can uplift marginalized voices in your community by sharing the experiences of a neighbor, a friend or your abuela. By leaning on our collective and individual lived experiences, we can achieve an equitable healthcare system that leaves no one behind.
###
Ivelyse Andino is the award-winning telehealth founder and CEO of the first Latinx-owned Public Benefit Corporation in New York state, Radical Health, which is working to create an equitable medical system and empower underserved communities through healthcare fluency.










